My research team recently published the article Time-restricted feeding plus resistance training in active females: a randomized trial in The American Journal of Clinical Nutrition. This post attempts to provide both brief and extended summaries of the study, as well as provide a more detailed context for this study and answer some questions I have received.
*If you just want the take-home points, click here
*To stay caught up with my lab’s research, feel free to connect on social media: [do_widget id=acx-social-icons-widget-4]
Table of Contents
Brief Summary
Background
Time-restricted feeding (TRF) is a form of intermittent fasting that limits all daily food intake to a particular number of hours.
Our research group has previously published what I believe to be the first two controlled trials of TRF plus resistance training, both in male participants Tinsley et al. 2017, Moro et al. 2016). These articles generated substantial reader interest, as described in the background section of the extended summary on this page.
Our third trial, conducted in resistance-trained females, was recently published by the prestigious American Journal of Clinical Nutrition (on July 3, 2019). A brief overview of the new study is presented below.
Design
Our study randomly assigned resistance-trained females to one of three groups:
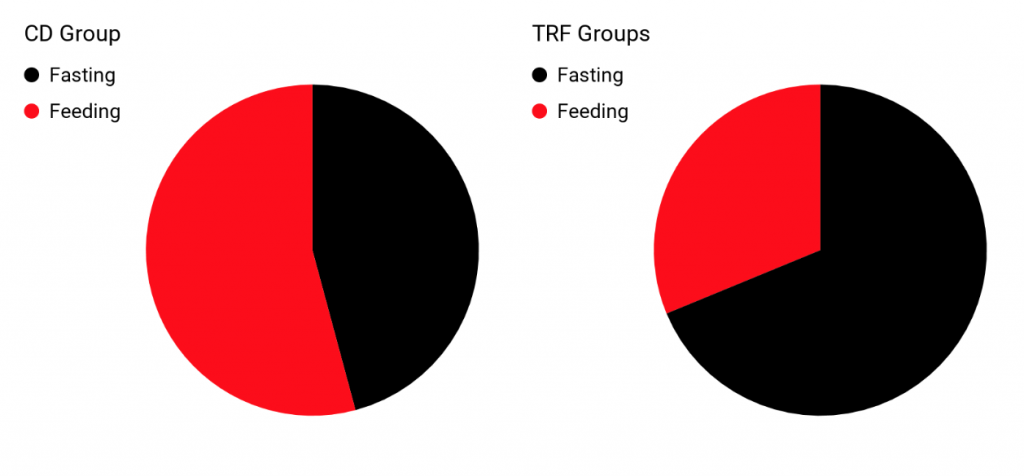
- CD: A control diet that required breakfast consumption. The actual duration of daily feeding in this group ended up being ~13 hours/day.
- TRF: A TRF group asked to consume all calories between 12:00 and 20:00 every day. The actual duration of daily feeding in this group ended up being ~7.5 hours/day.
- TRFHMB: A group that followed the same TRF eating schedule but also consumed supplemental beta-hydroxy beta-methylbutyrate (HMB), a metabolite of the amino acid leucine, during fasting periods. The actual duration of daily feeding in this group ended up being ~7.5 hours/day.
All groups were provided with whey protein supplements and achieved an average protein intake of 1.6 grams per kilogram of body weight per day.
All three groups followed the same supervised 8-week resistance training program, which was performed on 3 nonconsecutive days each week. Upper- and lower-body sessions were alternated throughout the study. The sessions were conducted in the afternoons, and the TRF groups were instructed to not exercise fasted.
Prior to beginning the intervention, as well as during the intervention, dietary intake was estimated from weighed diet records, and physical activity levels were objectively monitored via accelerometry.
At baseline and after 4 and 8 weeks of the study intervention, assessments of body composition, muscular performance, and a variety of physiological variables took place. An overview of the study visits and procedures is shown in the figure below.
Data were analyzed in two different ways. One way included all participants regardless of whether they dropped out or failed to comply with the protocol (this is called an intention-to-treat analysis). The other way included only participants who completed the whole study and also excluded some participants for falling below our compliance thresholds (this is called a per protocol analysis).
Results
While most results were similar between the intention-to-treat and per protocol analyses, there were a few notable differences, as described below.
Body weight changes were minor, with a change of 0 to +1% in the TRF groups and +2% in CD.
All groups increased fat-free mass, as assessed by a 4-component (4C) model, by 2 to 3% (2 to 3 pounds) relative to baseline. Additionally, all groups increased muscle thickness of the elbow flexor (i.e. biceps brachii and brachialis) and knee extensor (i.e. quadriceps femoris) muscle groups, with no differences between groups.
In the intention-to-treat analysis, there was no significant difference between fat mass changes in CD (+2%; ~1 pound), TRF (-2%; ~1 pound) or TRFHMB (-4%; ~1.5 pounds). In the per-protocol analysis, significant differences between groups were observed. Both TRF and TRFHMB exhibited fat loss as compared to CD at the week 4 time point. However, by the end of the study, only changes in TRFHMB were statistically significant. The final changes in fat mass in the per protocol analysis were +2% (~1 pound) for CD, -4% (~1.75 pounds) for TRF, and -7% (~3 pounds) for TRFHMB.
The results for both analyses can be seen below, with the intention-to-treat results shown on top and the per protocol results shown on bottom.
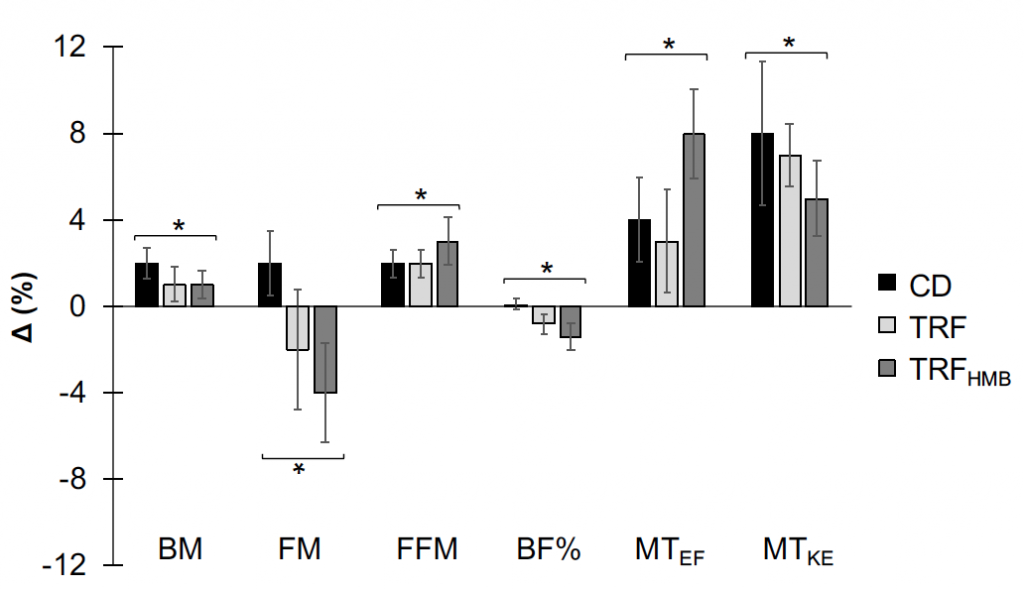
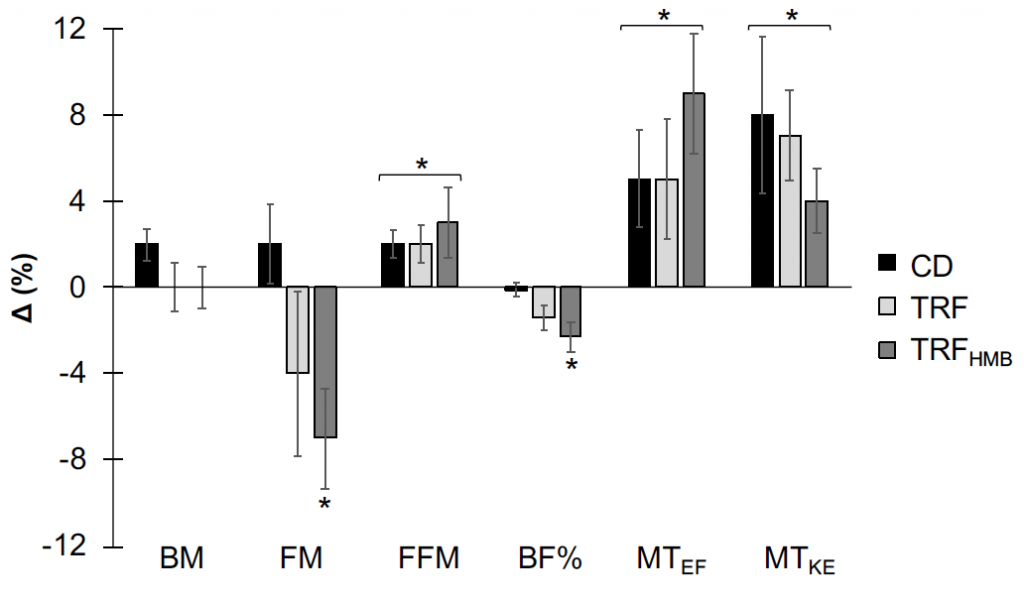
In both figures, percent changes (mean ± SE) are displayed as differences between week 0 (W0) and week 8 (W8) values relative to W0 values for each variable. Asterisks with brackets indicate significant changes in all groups (i.e. time main effects), with non-significant differences between groups. Asterisks above only one column indicate a change in only the specified group. BF%: 4- component model body fat percentage; BM: body mass; CD: control diet; FM: 4-component model fat mass; FFM: 4-component model fat-free mass; MTEF: ultrasound muscle thickness of elbow flexors; MTKE: ultrasound muscle thickness of knee extensors; TRF: time-restricted feeding; TRFHMB: time-restricted feeding plus HMB supplementation.
Muscular performance improved in all groups, without significant differences between groups. Results from the intention-to-treat analysis are shown below, and results in the per protocol analysis were similar.
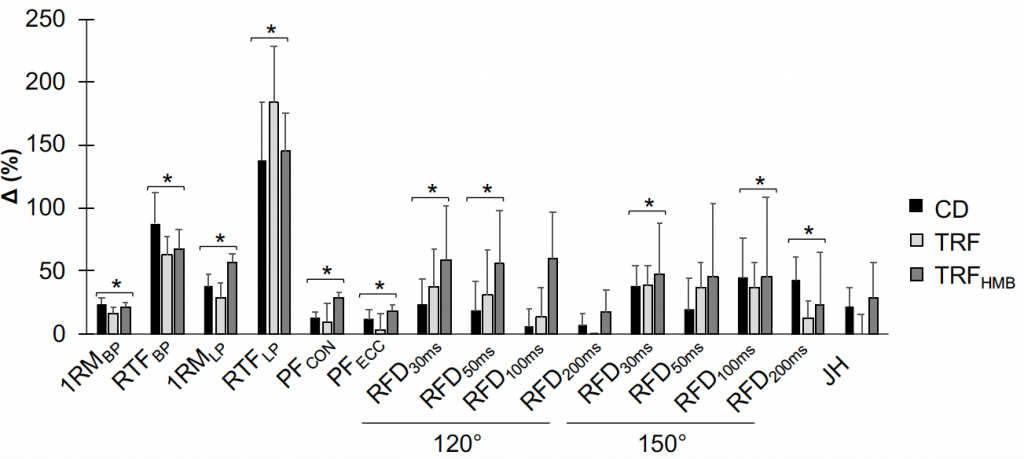
Percent changes (mean + SE) displayed as differences between week 0 (W0) and week 8 (W8) values relative to W8 values for each variable. Asterisks with brackets indicate significant changes in all groups (i.e. time main effects), with non-significant differences between groups. Muscular strength and endurance were evaluated on the leg press and bench press exercises, peak forces were obtained from isokinetic squat testing, rate of force development was obtained from isometric squat testing, and jump height was calculated using force platforms. 120º: 120º knee angle for isometric squat testing; 150º: 150º knee angle for isometric squat testing; 1RMBP: 1-repetition maximum on bench press; 1RMLP: 1-repetition maximum on leg press; CD: control diet; JH: jump height; PFCON: peak concentric force on mechanized squat; PFECC: peak eccentric force on mechanized squat; RFD: rate of force development (durations over which RFD values were calculated are shown in subscripts); RTFBP: repetitions to failure on bench press; RTFLP: repetitions to failure on leg press; TRF: time-restricted feeding; TRFHMB: time-restricted feeding plus HMB supplementation.
No significant changes in physiological variables occurred in any groups.
Minimal side effects were observed, and questionnaire responses indicated that mood improved and uncontrolled eating decreased across time in all groups.
Closing Thoughts
Our study demonstrated that comparable improvements in fat-free mass, muscle thickness, and muscular performance can be achieved with dramatically different feeding schedules (eating over the course of ~7.5 hours/day as compared to ~13 hours/day), provided that both groups are consuming a similar number of calories and sufficient protein (1.6 g/kg).
In addition to exhibiting no impairment of fat-free mass accretion or muscular performance improvement, both TRF groups exhibited a small amount of fat loss when only those who completed the whole study were considered. As such, it appears that TRF with a relatively high protein diet plus resistance training is a suitable strategy for concurrent muscle gain and fat loss.
Although a number of prior studies have demonstrated improvements in physiological variables, those examined in the present study were generally unchanged. This may be partially attributable to the healthy, active population. Although our previous work (Moro et al. 2016) did demonstrate some beneficial improvements in inflammatory markers and other variables in an active population, as well as a small decrease in testosterone, these variables were not specifically examined in the present study due to resource limitations.
Despite a theoretical rationale for benefits of HMB during periods of reduced energy intake, such as fasting, HMB consumption did not definitely improve results in the present study. However, the greater fat loss with HMB consumption in the per protocol analysis may be worthy of additional investigation.
In the present study, very minimal dietary advice was provided beyond the assigned eating window. TRF, as implemented in the present study, represents a very simple dietary strategy to support improvements in body composition in exercising individuals. However, the ease of adherence to TRF likely varies between individuals, and it is not recommended for everyone.
Extended Summary
Background
Intermittent Fasting
Intermittent fasting (IF) has sustained a high level of popularity for several years.
Although narrower definitions are often circulated, I consider IF to be a broad term for eating patterns with regularly occurring periods of fasting (i.e. ingesting no calories) for longer than a typical overnight fast (Tinsley et al. 2015).
Within this umbrella term, one of the more popular forms of IF is time-restricted feeding (TRF). This is the form that essentially dictates a daily “feeding window,” often 4 to 10 hours in duration, during which all daily calories are consumed. The remaining hours each day are a “fasting window,” during which no calories are consumed.
Perhaps the most common implementation of TRF is an 8-hour feeding window, often observed from midday until the evening.
While much of the existing IF (and TRF) research has focused on obesity and chronic disease risk, there is substantial interest in the potential applications of these programs in healthy, exercising individuals.
We (my research collaborators, namely Antonio Paoli, and myself) have previously published what I believe to be the first two controlled trials of IF plus resistance training (Tinsley et al. 2017, Moro et al. 2016).
Recently (July 3, 2019), we published the results of our third trial of TRF plus resistance training, this time in active female participants.
This extended summary will present some background regarding our previous work in this area, provide an overview of our new study, and answer questions some readers may have.
Our Previous Studies
The citation information for our two previous TRF plus resistance training studies is shown below.
Tinsley GM*, Forsse JS, Butler NK, Bane AA, La Bounty PM, Morgan GB, Grandjean PW. Time-Restricted Feeding in Young Men Performing Resistance Training: A Randomized Controlled Trial. European Journal of Sport Science (2017) 17(2): 200–207.
Moro T, Tinsley G, Bianco A, Neri M, Battaglia G, Palma A, Paoli A*. Effects of Eight Weeks of Time-restricted Feeding on Basal Metabolism, Maximal Strength, Body Composition, Inflammation, and Cardiovascular Risk Factors in Resistance-trained Males. Journal of Translational Medicine (2016) 14: 290.
Tinsley et al.
I led the Tinsley et al. study as a doctoral student at Baylor University. Due to limited resources (i.e. zero money for the project and limited personnel to assist), this was a fairly basic study employing a less common TRF variation in recreationally-active males.
Participants were randomized to TRF or a control diet with no restrictions. The TRF program consisted of following a 4-hour feeding window on 4 days per week, while having unrestricted food intake on the other 3 days each week. Both groups performed an 8-week resistance training program, which alternated between upper and lower body sessions. Four sets of 8 to 12 repetitions were performed for each exercise, with 90 seconds of rest between sets, and participants were asked to train to volitional failure. The resistance training program was performed on the 3 non-fasting days each week for the TRF group.
The major results were: (1) Although not statistically significant, there was an apparent attenuation in lean mass gains with TRF (−0.2 kg; effect size [d] = −0.02) compared with the control group (+2.3 kg; effect size = 0.25), although both groups increased muscle cross-sectional area with no differences between groups; (2) There were no statistically significant differences in fat mass changes between TRF (-0.6 kg; effect size = -0.07) and the control diet (+0.8 kg; effect size = 0.18); and (3) equivalent improvements in muscular performance (strength and endurance on the bench press and leg press exercises) were observed.
A couple major items to note were that we provided no instruction beyond the feeding window, the TRF group self-selected a lower protein intake (1.0 g/kg) than the control group (1.4 g/kg), and due to the previously mentioned limitations, the RT program was not directly supervised (although participants were monitored weekly).
Despite some of these notable limitations, the article generated a fair bit of interest due to the very limited information in this area. In fact, it is currently ranked in the 99th percentile of all research indexed by Altmetric, a site which quantifies the attention research articles receive.
This paper received a decent amount of criticism online, some of it fair, due to some of its notable limitations. However, it was awarded the 2018 Best Paper Award by the European Journal of Sport Science.
Moro et al.
While the success of the Tinsley et al. article was a nice accomplishment for the research team, it pales in comparison to the other work (Moro et al.), which was led by my collaborator Dr. Antonio Paoli at the University of Padova in Italy.
This trial examined the very popular “LeanGains” form of IF, which is essentially TRF with an 8-hour feeding window.
This article’s Altmetric “attention score” is currently in the top 5,000 out of >13 million indexed research items (i.e. the top 0.04%), regardless of article age.
It has been accessed > 120,000 times on the publisher’s website in less than 3 years, along with >11,000 reads on ResearchGate and who knows how many views in PubMed Central.
I mention all of this just to say that our prior articles, and the Moro et al. study in particular, have garnered substantial attention. It seems that both the scientific community and the general well-informed population have an interest in research in this area.
In the Moro et al. study, well-trained male participants (average age of ~29, weight of ~84.5 kg [~186 pounds], body fat percentage of ~13%) were randomized to TRF with an 8-hour feeding window each day or a control diet with a ~13 hour feeding window.
Both groups were prescribed 3 meals per day, plus a 20 grams of whey protein post-exercise. In the control group, meal times were set at 8 AM, 1 PM, and 8 PM. In the TRF group, meal times were set at 1 PM, 4 PM and 8 PM.
Both groups maintained habitual calorie and macronutrient intake, which consisted of ~3,000 calories/day, ~1.9 g/kg/day of protein, ~4.5 g/kg/day of carbohydrate, and ~0.9 g/kg/day of fat, on average.
The supervised resistance training program followed by both groups was a 3 day/week split routine (chest/biceps, legs/shoulders, back/triceps). The training protocol involved 3 sets of 6–8 repetitions at 85 to 90% of the 1RM, and repetitions were performed to failure with 180 seconds of rest between sets and exercises
Bench press and leg press strength were maintained in both groups. The slight increases observed in both groups were not statistically significant. This is not surprising given the relatively short duration of the study (8 weeks), the training status of the participants, and the fairly straightforward resistance training program.
However, reductions in body mass and fat mass were observed in the TRF group. The fat loss in the TRF group was ~16%, with a non-significant decrease of ~3% in the control group. While the fat loss in the TRF group may sound large, it is important to remember that the participants were lean to begin with (~13% body fat), meaning that the absolute changes weren’t enormous (~1.6 kg or ~3.5 pounds).
No changes, or differences between groups, in fat-free mass were observed. Both groups had a non-significant increase of less than 1% of baseline fat-free mass.
Leg press strength increased in both groups, while bench press strength was maintained.
There were also differential effects between groups for several physiological variables:
- Total testosterone and IGF decreased in the TRF group, but not the control group. For context, the decrease in the TRF group was from ~21 nmol/L to ~17 nmol/L, and the reference range would be something like ~10 to ~35 nmol/L.
- Blood glucose, insulin, and HOMA-IR decreased in TRF only
- Adiponectin increased in the TRF group only.
- Letpin decreased in the TRF group, but not when normalized for fat mass
- Triglycerides decreased in the TRF group only, but other blood lipids did not change.
- The inflammatory markers TNF-α and IL-1β decreased in the TRF group only
- The respiratory quotient decreased in TRF only, indicating a shift towards greater reliance on fat oxidation for resting metabolism.
Based on self-reported diet records, energy intake was 91 calories per day lower in the TRF group (this was not a statistically significant difference). While I have read a number of write-ups of our study that point to this as the definitive answer for the differential physiological changes observed, this is not knowable from our experiment. Due to the pervasive and well-documented limitations of self-reported intake, we can’t know the exact dietary intake in this study. What’s more, this holds true for any study that is not conducted in a metabolic ward. Even if all food was provided to participants for an entire study, you don’t know what they are really doing. They could be throwing away the food you give them and heading to their favorite restaurant, and you would never know. Only if you have complete control of everything that is eaten, and there are no opportunities for “cheating,” can you truly know exactly what was consumed in a nutrition study. Even with very competent researchers and well-intentioned participants, you have to be extremely cautious about putting too much weight into the results of self-reported intakes.
A Few Final Notes
Although there were a number of similarities between our new study and the previous trials, there are some notable differences. I want to highlight two of them before diving into the design of this trial.
First, as both of the previous studies were conducted in male participants, I have been planning to conduct a follow-up trial in females for some time. There is a small amount of data indicating there could be sex differenes in response to some forms of IF (e.g. Heilbronn et al. 2005). I have seen a number of people speculating that IF could be problematic for females. However, the lack of data in the context of healthy, active individuals indicated that actual research needed to be done.
Second, the new study actually incorporated a third group. In addition to the TRF and control groups, there was a group that performed TRF but also ingested beta-hydroxy beta-methylbutyrate (HMB) supplements when they were fasting. While HMB has shown possible benefits in specific contexts, including certain clinical conditions and energy-restricted individuals, additional work that has come out since the design of this experiment casts doubt on its benefits in healthy, exercising individuals. However, the consumption of HMB as opposed to nothing, during the fasting periods of a IF program, does represent a unique context in which to evaluate this supplement. My original interest in HMB in the context of fasting arose from its purported anti-catabolic actions. We previously conducted a study of HMB free acid supplementation during acute 24-hour fasting (Tinsley et al. 2018), although this did not reveal benefits on the marker of muscle catabolism we investigated.
With all that background information out of the way, here is an overview of our newly-published study.
The New Study (Tinsley et al. 2019, AJCN)
This study was first published online in the American Journal of Clinical Nutrition on July 3, 2019. I paid to make this article open access, meaning it is freely available to everyone at https://doi.org/10.1093/ajcn/nqz126.
I will present some basic information regarding the study design, participants, and intervention below. However, I refer readers to the full article for details of our methodology.
Design
This study employed a reduced factorial design. In this case, this means that we used 3 out of 4 possible group combinations, as shown below:
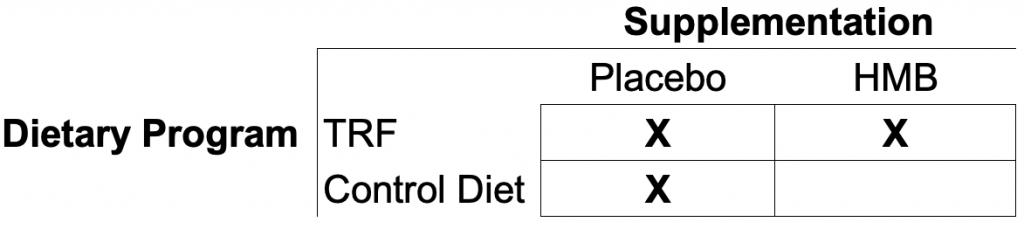
The reason for not having a fourth group was primarily due to the amount of funding available to conduct the study and the timeline for study completion. The absence of this group limits the number of possible comparisons we can make, but we selected the included groups based on our primary interests for this study (i.e. TRF versus a control diet, as well as whether supplemental HMB influenced the effects of TRF).
Participants
The participant characteristics can be seen in the table below. The main points are that all groups contained relatively young adult females with ~5 years of resistance training experience, on average, and current resistance training at a frequency of ~3 times per week. With that said, we did observe a variety of actual training statuses. As anyone who has spent time in the gym knows, there are a host of factors that contribute to someone’s true training status. You could have someone who has followed an intense, evidence-based program for 1 year who is more trained than someone who has dinked around in the gym for 5 years. All that to say, while the participants were resistance-trained, some had more room for improvement than others. With that said, there were no baseline differences for muscular performance between groups, indicating that we had an even distribution of true training statuses among the three groups.
Randomization and Groups
Participants were stratified (separated) based on two items prior to being randomly assigned to a group. These factors were 1) body fat percentage and 2) habitual breakfast consumption. Since both an individual’s baseline body composition and whether or not they typically eat breakfast could potentially influence adaptations to a TRF program, we wanted to make sure we had an even distribution of lower/higher body fat percentages and breakfast consumers/skippers in both groups. Taking these factors into account helped ensure that our groups were similar at the beginning of the study (which they were).
After taking these factors into account, participants were randomized into one of three groups using random integer sequences:
- The control diet (CD), which required breakfast consumption as soon as possible after waking. The actual feeding period ended up being ~13 hours on average.
- TRF, with an 8-hour feeding period from noon to 8 PM. The actual feeding period ended up being ~7.5 hours/day.
- TRFHMB, with an 8-hour feeding period from noon to 8 PM and 3 g/d HMB consumption during the fasting period. The actual feeding period ended up being ~7.5 hours/day. The HMB supplement was split into 1 gram doses consumed upon waking, mid-morning while still fasted, and before bed.
Importantly, both the CD and TRF groups took placebo capsules daily, and each supplement had a unique code so that the researchers wouldn’t accidentally learn which TRF group was consuming placebo capsules based on the CD group’s supplement code. Without giving capsules to all groups, the groups not receiving capsules could have felt that they weren’t getting the “special sauce,” and this could have affected their willingness to put forth effort in the program to which they were assigned.
A visual comparison of the duration of daily feeding and fasting periods is shown below.
Resistance Training Program
Participants in all groups completed the same 8-week resistance training program. This program was completed under researcher supervision in our Human Performance Laboratory. The program design is shown in the table below.
As shown, participants alternated between 4 different workouts (2 upper body and 2 lower body). For each set, participants were instructed to reach momentary muscular exhaustion within the specified repetition range. The specific exercises and variations chosen were partially based on equipment availability in our Human Performance Laboratory.
Participants were asked not to perform any other resistance training or high-intensity exercise outside of the study intervention. However, due to the difficulty in monitoring and enforcing limitations on outside activity, we employed objective physical activity monitoring through accelerometry.
Overview of Study Visits
A visual overview of the study visits and intervention is shown below.
The manuscript has a large amount of detail regarding the methods. Below, I will briefly describe a few of the methods I think are most likely to interest readers: body composition assessment, muscular performance assessment, and dietary monitoring.
Diet and Physical Activity Monitoring
Prior to beginning the intervention, as well as during the intervention, dietary intake was estimated from weighed diet records, and physical activity levels were objectively monitored via accelerometry.
As stated in the manuscript, and in the background information earlier in this article, substantial caution should be used when interpreting any form of self-reported dietary intake. While I believe that the use of food scales likely improved the accuracy of our dietary information, the dietary intake results shouldn’t be over-interpreted. Additionally, I suspect that behavioral modification (i.e. choosing to eat healthier) on diet tracking days could have occured, despite us specifically asking participants to eat normally.
Laboratory Assessments
The major variables assessed in this study were:
- Body Composition
- Whole-body composition assessed by rapid 4-component model (which required assessments via dual-energy x-ray absorptiometry and bioimpedance spectroscopy)
- Muscle thickness of upper and lower body muscle groups assessed by ultrasonography
- Muscular performance
- Muscular strength assessed by traditional 1-repetition maximum on the barbell bench press and angled leg press (hip sled) exercises
- Muscular endurance assessed by repetitions to failure, using 70% of the baseline 1-repetition maximum, on the barbell bench press and angled leg press (hip sled) exercises
- Maximal concentric and eccentric force production from isokinetic testing using a mechanical squat device
- Maximal isometric force production and rate of force development at two different knee angles using a mechanical squat device
- Vertical jump performance as assessed using force platforms
- Physiological Variables
- Resting metabolic rate and substrate utilization assessed using indirect calorimetry
- Vascular function (pressures, heart rate, pulse wave velocity) assessed using applanation tonometry
- Standard blood markers (glucose, cholesterol, HDL, triglycerides, VLDL, insulin, and LDL) assessed at a clinical laboratory
- The salivary cortisol awakening response assessed at a clinical laboratory
- Questionnaires for mood, eating behaviors, sleep quality, and side effects
As stated previously, I refer interested readers to the full article for more methodological details.
Data Analysis
While the manuscript contains the details of our analysis methods, there is one point worth I would like to explain. We performed all of our analysis using two frameworks. The first, which is the primary one presented in the manuscript, is called an intention-to-treat (ITT) framework. A simple definition of ITT is:
“A strategy for analyzing data in which all participants are included in the group to which they were assigned, whether or not they completed the intervention given to the group. Intention-to-treat analysis prevents bias caused by the loss of participants, which may disrupt the baseline equivalence established by random assignment and which may reflect non-adherence to the protocol.”
CONSORT
ITT analysis is generally favored in clinical trials for the reasons mentioned above, among others (BMJ 2010). The other framework, which includes only participants who completed the trial and complied with the study intervention, is the per protocol (PP) analysis. While the ITT analysis was favored in the manuscript, the full PP results are available in the supplementary material for the article.
In our study, 40 participants began the trial and were included in the ITT analysis. In the PP analysis, the 24 participants who completed the whole trial and exhibited compliance above our specified thresholds were included.
The ITT analysis dominates the manuscript, based on current recommendations and the guidance of the editors at AJCN, I do want to mention that you could make an argument for the importance of the PP analysis, as it addresses the effects in those who actually completed the whole program and adequately adhered. The PP analysis is expected to have larger effects for these reasons, and this is what we observed in the present study. Despite some differences in magnitude of effects, the results of the PP and ITT analyses were very similar, with one notable exception (body fat changes, as described in the results section below).
Major Results
Note 1: We examined a large number of variables in this study. In addition to all the information presented in the manuscript, there are 17 supplemental tables and 2 supplemental figures, which are freely available online. I will only mention a few major points here, but interested readers interested in more detail are directed to the manuscript.
Note 2: While most results were similar between the intention-to-treat and per protocol analyses, there were a few notable differences (primarily for body fat).
TRF Program vs. Control Diet
Prior to the study, all groups averaged a ~9.5 to 11 hour daily feeding window. During the intervention, both TRF groups had a ~7.5 hour feeding window, with the control group following a ~13 hour feeding window.
Prior to the study, all groups averaged ~4 to 4.5 eating occasions per day. During the study, the TRF groups averaged ~4.5 eating occasions per day, and the CD group averaged just over 5 per day. Note that consuming the prescribed protein shakes counted as an eating occasion.
There were no significant differences between the groups for any dietary intake variables (i.e. calorie and macronutrient consumption).
All groups reported energy intake lower than what we originally intended to prescribe ([1.5 x REE] – 250). Energy intake actually increased in all groups during the intervention, of a similar magnitude to the energy content of the protein supplement (~200 to 250 kcal/d). Of course, as in any studies conducted outside of a metabolic ward, there is a distinct possibility of errors in the diet records. We did employ weighed diet records, meaning we provided food scales to all participants to use for quantity recording, but the observations of underestimation of energy intake are consistent and pervasive. Additionally, although participants were asked to not alter their eating habits on days they tracked, there is also a distinct possibility of intentional or unintentional behavioral modification on tracking days.
Even with the possible underestimations of energy intake, protein intake increased in all groups (from ~1.2 g/kg/day at baseline to ~1.6 g/kg/day during the intervention). This intake is consistent with recommendations for muscular hypertrophy in active individuals (X). Additionally, it is possible protein intake could have been higher if either behavioral modification or tracking errors occurred on days when the diet was recorded.
Carb intake was between 2 and 3 g/kg/day, and fat intake was ~1 g/kg/day during the intervention in all groups.
Body Composition
Body weight changes were minor, with a change of 0 to +1% in the TRF groups and +2% in CD.
All groups increased fat-free mass, as assessed by a 4-component (4C) model, by 2 to 3% (~2 to 3 pounds) relative to baseline. Additionally, all groups increased muscle thickness of the elbow flexor (i.e. biceps brachii and brachialis) and knee extensor (i.e. quadriceps) muscle groups, with no differences between groups.
In the intention-to-treat analysis, there was no significant difference between fat mass changes in CD (+2%; ~1 pound), TRF (-2%; ~1 pound) or TRFHMB (-4%; ~1.5 pounds). In the per-protocol analysis, significant differences between groups were observed. Both TRF and TRFHMB exhibited fat loss as compared to CD at the week 4 timepoint. However, by the end of the study, only changes in TRFHMB were statistically significant. The final changes in fat mass in the per protocol analysis were +2% (~1 pound) for CD, -4% (~1.75 pounds) for TRF, and -7% (~3 pounds) for TRFHMB.
The results for both analyses can be seen below, with the intention-to-treat results shown on top and the per protocol results shown on bottom.
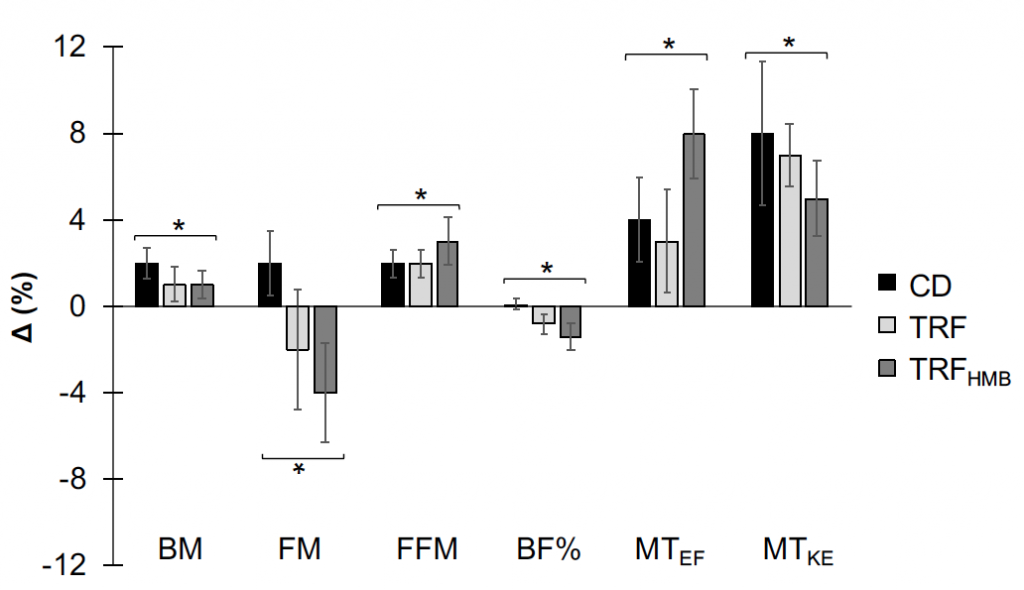
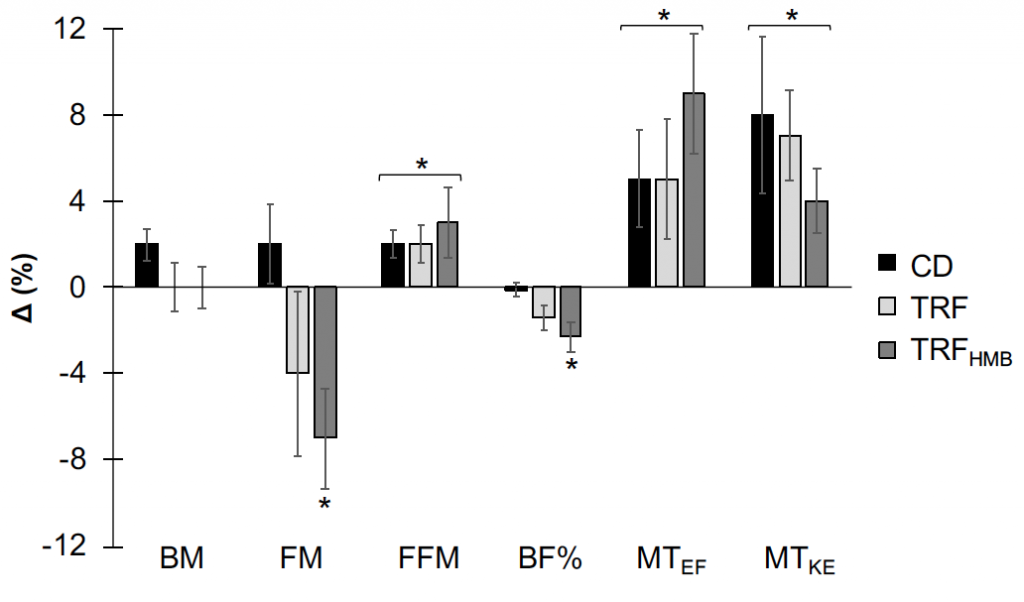
In both figures, percent changes (mean ± SE) are displayed as differences between week 0 (W0) and week 8 (W8) values relative to W0 values for each variable. Asterisks with brackets indicate significant changes in all groups (i.e. time main effects), with non-significant differences between groups. Asterisks above only one column indicate a change in only the specified group. BF%: 4- component model body fat percentage; BM: body mass; CD: control diet; FM: 4-component model fat mass; FFM: 4-component model fat-free mass; MTEF: ultrasound muscle thickness of elbow flexors; MTKE: ultrasound muscle thickness of knee extensors; TRF: time-restricted feeding; TRFHMB: time-restricted feeding plus HMB supplementation.
Muscular Performance
ITT results are shown on top, and PP results are shown on bottom. While the statistical significance of some variables differed, the results were generally the same. The big-picture result was that muscular performance improved notably in all groups, without significant differences between groups.
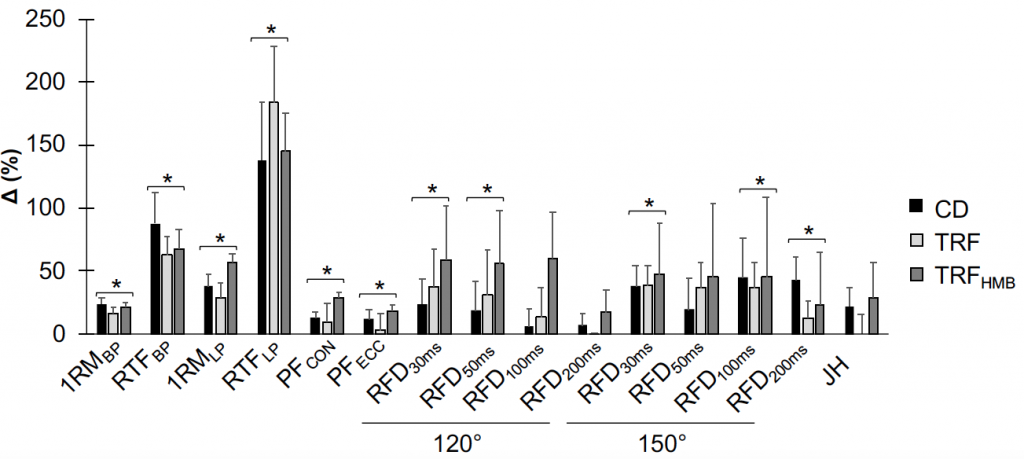
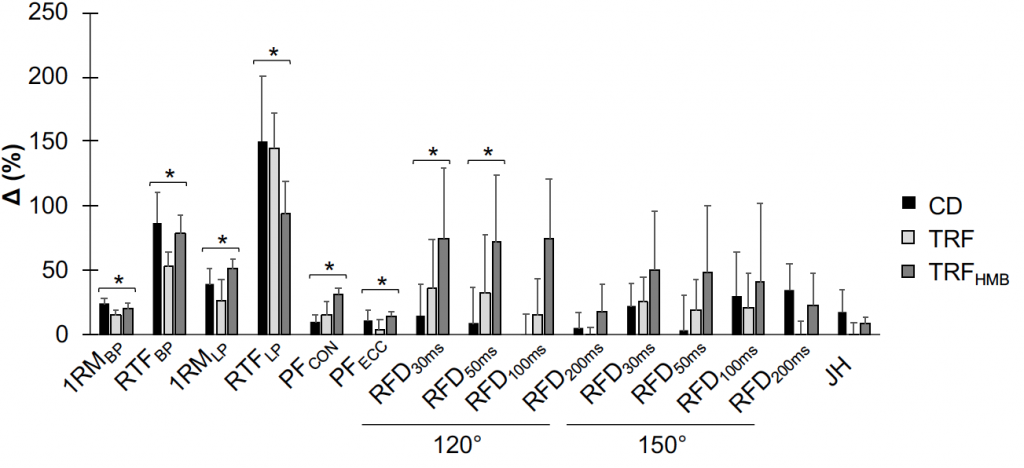
Percent changes (mean + SE) displayed as differences between week 0 (W0) and week 8 (W8) values relative to W8 values for each variable. Asterisks with brackets indicate significant changes in all groups (i.e. time main effects), with non-significant differences between groups. Muscular strength and endurance were evaluated on the leg press and bench press exercises, peak forces were obtained from isokinetic squat testing, rate of force development was obtained from isometric squat testing, and jump height was calculated using force platforms. 120º: 120º knee angle for isometric squat testing; 150º: 150º knee angle for isometric squat testing; 1RMBP: 1-repetition maximum on bench press; 1RMLP: 1-repetition maximum on leg press; CD: control diet; JH: jump height; PFCON: peak concentric force on mechanized squat; PFECC: peak eccentric force on mechanized squat; RFD: rate of force development (durations over which RFD values were calculated are shown in subscripts); RTFBP: repetitions to failure on bench press; RTFLP: repetitions to failure on leg press; TRF: time-restricted feeding; TRFHMB: time-restricted feeding plus HMB supplementation.
I don’t want to over-interpret the apparently disparate magnitude of changes, but a few things are worth noting:
An examination of effect sizes indicated potentially disparate improvements between groups for measures related to rapid force generation in the lower body, including 1RM for the leg press, peak concentric and eccentric forces on the mechanized squat device, and rate of force development. In both the ITT and PP analyses, the average effect size for these variables was 0.6 to 0.7 in TRFHMB as compared to 0.3 to 0.4 in CD and TRF.
There were potentially disparate changes in vertical jump height, with nice improvements in the CD and TRFHMB groups, but not TRF. In the ITT analysis, both CD and TRFHMB improved by 22 to 29% (effect size of 0.63 to 0.65), while there was zero change (literally zero) in the TRF group.
Other Variables
As a reminder of all the other variables that we assessed, here is the index of supplemental tables for this manuscript (yes, there are 17 supplemental tables for this manuscript):
The vast majority of these variables were not definitively changed by the intervention, and different effects between groups were not observed (with minor exception for select physical activity variables, as explained in the manuscript).
While this absence of statistical significance is worth mentioning, we also present % changes and effect sizes for all of these variables. Examination of these items may be interesting to some readers and could even provide ideas for future experiments.
Although changes in resting energy expenditure did not significantly differ between groups, the values observed in the ITT analysis were:
- CD group: -71 kcal/d (-5%); effect size = -0.42
- TRF group: -54 kcal/d (-3%); effect size = -0.33
- TRFHMB group: +15 kcal/d (+1%); effect size = +0.09
Based on this, there were certainly no adverse effects of resting metabolism as a result of truncating the feeding window, and the largest magnitude of decrease was observed in the CD group.
Closing Remarks
The discussion section of the manuscript should be very readable to most people who are actually reading this post. As such, I will largely refer you there.
However, a few of the major takeaways of the study are:
- Equivalent increases in lean mass, muscle thickness, and exercise performance were observed with dramatically different feeding schedules (eating over the course of ~7.5 hours/day as compared to ~13 hours/day) in trained female participants, when both feeding programs contained a similar number of calories and sufficient protein. This finding does not support the common contention that meals and protein intake must be spread out evenly over the entire day to support exercise adaptations.
- Both TRF groups exhibited a small amount of fat loss, as compared to a small amount of fat gain in the control group. The effects were not large and differed in statistical significance between our analyses, but this is noteworthy because of the simplicity of the dietary program and the very minimal dietary instruction provided to participants in the study. As such, it appears that TRF in combination with weight training may be a suitable strategy for active individuals wanting to simultaneously increase lean mass and lose body fat.
- Physiological variables, including blood markers, metabolic rate, vascular function, and more, did not change or differ between groups. While there could be unique health benefits of intermittent fasting in certain populations, we did not see clear benefits in this sample of relatively young, healthy, and active participants. Of course, we did not quantify all physiological variables, so beneficial or detrimental effects could have occurred that we did not detect.
- HMB did not definitely improve outcomes in this study, although fat loss was greater with HMB supplementation when only individuals who completed the whole study were evaluated (i.e. the per protocol analysis). Possibly greater magnitudes of improvements for metrics of rapid force production of the lower body were observed, but these were not definitive.
- Minimal side effects were observed with this program. However, a very small number of participants reported greater hunger, irritability, or fatigue when following the TRF program. Based on this, and common sense, it is likely that TRF (and IF in general) is not ideal for certain individuals. Since adherence is known to be one of the most critical factors for long-term success with a dietary program, IF is probably not a good strategy for those who find it especially difficult. With that said, a number of our participants reported that the TRF program got substantially easier after they had followed it for several days or weeks.
Q&A
Why did you bother writing up a summary of your article?
I have seen our previous articles written about, commented on, and discussed online for the past couple years. While some of these were reflective of what we actually reported, others were not. This time, I figured that it may be beneficial to provide my own perspective since I have spent an enormous amount of time on this project over the course of 2 years.
Why didn’t you do _____? Why didn’t you control for _____?
Anyone who hasn’t designed and completed a clinical trial in humans may not understand the tremendous number of challenges encountered in a project like this. To state it succinctly, we did the best we could with the resources we had. I led the study and had several other faculty members that assisted with specific components. This data collection occurred prior to the approval of my department’s PhD program, so there were no PhD students (or postdocs) to assist with the project. I did have a terrific team of ~12 undergraduate and master’s students, but this was a very large project to complete with the resources that were available. In addition to personnel constraints, there are of course financial and time constraints that prevented us from doing everything we would have liked. Nonetheless, my goal was to get the maximal amount of information from our intervention, and I do feel that we accomplished this.
Why was HMB supplementation part of this study? Why doesn’t the title mention HMB? Why isn’t HMB discussed more?
I am aware that there has been controversy surrounding HMB studies within the last few years and that the inclusion of HMB in this study could raise eyebrows of some within the sports nutrition research community. My reasons for including a HMB group were:
- A genuine interest in whether HMB would have utility in this unique context (i.e. it was consumed during fasting periods during which nothing would otherwise be consumed).
- To follow up on a previous acute study of HMB supplementation during 24-hour fasting.
- Because the study sponsor was willing to provide funding for the study. As any tenure-track professor at a major research university knows, it is pretty much imperative to obtain external funding in order to successfully gain tenure and promotion. Because of this, I honestly may not have been able to justify investing such an enormous amount of time and effort into this project if I was not receiving any funding. With that said, it is worth noting that a relatively large portion of the study costs were funded from my own start-up funding (i.e. from Texas Tech).
The answer to the last two questions is “because of the journal requirements.” As other researchers know, each journal has its own set of author guidelines which must be followed. Due to the limits of words in the title, introduction, and discussion, I had to keep several parts of the manuscript more concise that I would have liked. This is the primary reason for a relatively limited discussion of HMB, or other topics, in these sections.
What is the 4-component model that was used to assess body composition?
The 4-component model (4C; also known as 4-compartment model) splits all body mass into water, fat, bone, and “residual,” which primarily contains protein, glycogen, and minerals dissolved in body fluids. Even though all these components have been taken into account, the body composition estimates are typically reduced back to simple estimates of fat mass (FM) and fat-free mass (FFM). The benefit of multi-compartment models like this is that they have “taken more things into account” when generating a body fat percentage estimate. The form of the 4C model we used is called the “rapid” 4C and can be produced from dual-energy x-ray absorptiometry (DXA) output, along with estimates of body water. For water, we used bioimpedance spectroscopy (BIS). Unlike most bioelectrical methods, which use regression/prediction equations to estimate body fluids, BIS utilizes mathematical modeling to predict fluid volumes using an individual’s raw electrical data. As such, some believe it is a superior bioelectrical method for fluid estimation.
In the manuscript, why are the introduction and discussion so short, but the methods so long?
This was the case due to journal requirements. AJCN would only allow 1.5 pages (in the Word document) for the introduction and 4 pages for the discussion. These limits were very challenging due to the large number of items examined in this study. While I was not able to fully discuss all the data we present, my goal was to provide all relevant data via the manuscript and supplemental materials online.
Why did you pay to make this open access?
I didn’t want a paywall to be a barrier to any interested person. It cost me $3,000 out of my lab budget to make the article open access, as well as another ~$2,000 in page charges for the journal. While I don’t have the budget to do this for every article, I felt that it was worth it for this one in order to allow free access to everyone.
How can I stay caught up with your research?
I typically post about our new research online, so feel free to connect on social media:
[do_widget id=acx-social-icons-widget-3]